Health Anxiety in Medical Settings: A Clinician-Friendly Update You Should Know About
A new version of the Short Health Anxiety Inventory has been adapted for people with chronic illnesses. Here’s why it matters for your CBT practice.
Health anxiety can be difficult to navigate in therapy, especially when clients are also managing chronic medical conditions. While CBT offers effective strategies for managing illness-related worry, standard assessment tools like the Short Health Anxiety Inventory (SHAI) often fall short when applied in medical contexts.
Why? Because many of these clients aren’t worried about a hypothetical illness, they already have a diagnosis.
That’s where the Health Anxiety Inventory for Medical settings (HAI-M) comes in. A recent paper published in The Cognitive Behaviour Therapist Journal outlines the development and validation of this updated tool [1].
The HAI-M was designed to address a major gap in how we assess health anxiety in clients with chronic illnesses. For CBT professionals working in general practice, hospital settings, or integrated care, this update is worth knowing about.
The Problem with Standard Measures
The original SHAI has been widely used to assess health anxiety in the general population. It’s reliable and has solid psychometric properties [2]. But when administered to people who do have medical conditions, like chronic pain, multiple sclerosis, or ME/CFS, some of the questions can feel invalidating or off-base.
For example, asking whether someone is worried about becoming ill doesn’t quite fit when that person already has a diagnosis. And suggesting that bodily symptoms are being imagined can trigger defensiveness or disengagement. Clinicians often report that these tools feel like they’re pathologising normal concern [3].
The reality is, not all health-related worry is excessive. In clients managing chronic illnesses, a baseline level of concern or symptom monitoring may be appropriate, even necessary. But distinguishing between adaptive vigilance and clinically significant anxiety requires nuance, and the right tools.
When those tools aren't sensitive to context, the therapeutic relationship can suffer. Clients may feel misunderstood or dismissed. And practitioners may struggle to create a working formulation that explains the interplay between medical symptoms and cognitive processes. This is where the HAI-M fills an important clinical need.
The HAI-M: What Changed?
To address these concerns, researchers Colenutt and Daniels used a Delphi method with both clinicians and people living with chronic conditions to adapt the SHAI [1]. A Delphi method, for context, involves structured rounds of expert consultation aimed at reaching consensus on how to improve or design a measure.
The result is the 12-item HAI-M, which:
Removes or rewords items that imply illness is imagined or unfounded
Uses language that validates the presence of real symptoms
Retains core elements that measure health-related worry, reassurance-seeking, and preoccupation
Participants also found it more acceptable than the original SHAI, describing it as more reflective of their lived experience. This higher acceptability is a critical factor in health settings, where client dropout and therapeutic alliance are already areas of concern [4].
Unlike the SHAI, which was developed to assess health anxiety in the general population, the HAI-M was created with the voices of people with long-term conditions baked into its design. That alone sets it apart from most other measures in our toolbox.
How This Applies in Practice
Professionals working in health or mental health settings may already be familiar with the challenges of assessing health anxiety in medical populations. The HAI-M offers a practical, brief tool that can improve therapeutic alliance and help guide formulation.
In clinical use, the HAI-M can help:
Screen for health anxiety in clients with known diagnoses
Track symptom change over time
Clarify whether a client’s worry is proportionate or driven by cognitive distortions
Identify patterns that may benefit from targeted interventions such as behavioral experiments or cognitive restructuring
For example, a client with a long-term pain condition may score high on items related to worry or excessive checking. This can open up a discussion about patterns of reassurance-seeking, avoidance, or hypervigilance, all of which can be targeted with standard CBT techniques [5].
The HAI-M is especially useful in distinguishing between understandable concern about symptoms and health anxiety that is causing significant distress or functional impairment. It also supports more sensitive and collaborative treatment planning. Clients with chronic health conditions often report feeling misunderstood or dismissed by mental health providers. Using a measure that validates their experience while still helping assess the impact of anxiety can improve rapport and engagement.
The measure may also prove useful in multidisciplinary or stepped care settings. For example, being able to identify when symptom-related anxiety is contributing to increased GP visits or avoidant behavior can help improve coordination and outcomes. In health-focused CBT work, where brief intervention models are becoming more common, tools like the HAI-M help clinicians make quick but meaningful decisions about treatment priorities.
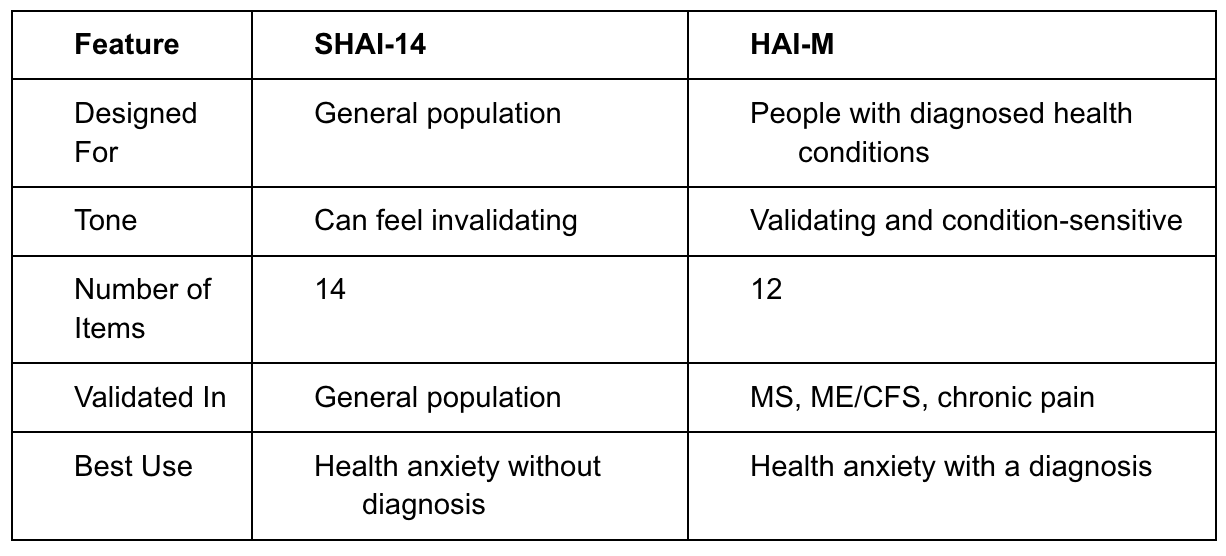
Comparing SHAI and HAI-M
One of the major advantages of the HAI-M is that it allows for greater clinical nuance. Rather than forcing practitioners to choose between dismissing valid medical concerns and pathologising adaptive behavior, it provides a framework for exploring the "excessive" part of health anxiety without denying the real challenges of living with chronic illness.
The removal of certain SHAI items that implied symptoms were imagined makes it more likely that clients will engage meaningfully with the questionnaire. The wording of HAI-M items encourages reflection rather than defensiveness, making it a better entry point into deeper therapeutic work.
In CBT settings where time is often limited, a tool that promotes buy-in while offering reliable, targeted information about symptom patterns is invaluable. The HAI-M enables clinicians to move beyond vague health-related concerns into structured intervention planning, all while maintaining a respectful, validating tone.
Using the HAI-M in Clinical Work
The HAI-M is brief and easy to administer, making it a good candidate for early assessment.
It can be used to:
Inform a collaborative CBT case formulation
Identify triggers and maintaining factors
Monitor change over time, particularly if health anxiety is a treatment target
In situations where health anxiety is suspected but not clearly articulated, the measure can help bring this into focus in a non-confrontational way. It supports a respectful and person-centred approach.
For clinicians newer to working in health psychology or physical health contexts, the HAI-M also functions as a guide. The structure and phrasing of items help cue clinicians into the cognitive and behavioral patterns worth exploring.
Additionally, services aiming to standardize health anxiety assessments across teams may find the HAI-M particularly useful. Its specificity for medical settings makes it easier to integrate into routine care, and its development process ensures it aligns with the lived realities of many patients [6].
Accessing the HAI-M
The HAI-M is available in full within the published article by Colenutt & Daniels [1]. It contains instructions for administration and scoring. While formal clinical cut-offs are still being validated, preliminary research has suggested that scores of 18 or above may indicate clinically significant health anxiety in medical populations [5]. Clinicians are encouraged to interpret scores alongside contextual clinical judgment.
Additionally, services aiming to standardise health anxiety assessments across teams may find the HAI-M particularly useful. Its specificity for medical settings makes it easier to integrate into routine care, and its development process ensures it aligns with the lived realities of many patients [6].
Moving Forward
Assessment tools shape how clients understand their own experiences. Using a measure like the HAI-M communicates that anxiety and physical illness are not mutually exclusive, and that both can be treated with care and skill.
Future research will likely establish clinical cut-offs, explore broader populations, and evaluate sensitivity to change post-treatment. But even now, the HAI-M is a step forward for those working to provide tailored, evidence-based support to people navigating health-related worries alongside chronic conditions.
This tool reflects a wider shift toward validating, context-sensitive approaches in CBT assessment. It respects the reality of physical illness while still giving clinicians the information they need to target maladaptive thought patterns and behaviors.
In an increasingly complex healthcare environment, tools that bridge the gap between medical and psychological needs are more essential than ever. The HAI-M shows that with thoughtful design and collaboration between clinicians and clients, our assessment tools can better reflect the lived experiences of those we support.
Share your thoughts:
Are you supporting clients who experience health anxiety alongside chronic illness? What approaches have you found helpful in this context?
Author: Kavya Suresh Kumar