Rumination-Focused CBT and Its Role in Treating Repetitive Negative Thinking
Understand how rumination functions and how RF-CBT can can disrupt it, helping clients move from overthinking to acceptance.
Repetitive negative thinking (RNT), a cycle of unhelpful mental repetition that includes both worry and rumination, is a core feature of many mental health difficulties. But how does it operate, and can Cognitive Behavioural Therapy (CBT) effectively target it? Increasingly, research suggests that it can, especially when adapted through Rumination-Focused CBT (Rf-CBT).
What Exactly Is Rumination?
Most people occasionally reflect on the past, but rumination goes far beyond reflection. It involves a repetitive, uncontrollable focus on negative thoughts, feelings, or past events.

As Stenzel et al. (2015) define it, rumination consists of “thoughts and behaviours that focus attention on one’s negative feelings.”
Across definitions, three key features emerge:
A focus on negative affect
Repetitive, persistent thinking patterns
Maintenance through negative reinforcement
In simple terms, rumination keeps people “stuck”, continually revisiting distressing experiences or regrets. Unlike worry, which tends to focus on future events and uncertainty, rumination is rooted in the past, sustaining cycles of low mood and self-criticism.
Neuroscientific findings have begun to map the brain mechanisms involved. Langenecker et al. (2023) identified reduced connectivity between the left posterior cingulate cortex and right inferior frontal gyrus in individuals with high rumination, patterns that appeared to shift following Rumination-Focused CBT, suggesting neural flexibility in response to treatment. This also suggests this is a real, neurological process, which can help shift shame from clients who blame themselves for their inability to stop.
Depressive Rumination: When Thinking Becomes a Trap
Nolen-Hoeksema (2000) described depressive rumination as persistent thinking about one’s symptoms of depression, an inward focus that maintains and intensifies low mood.
This may help explain why some individuals fail to respond to traditional CBT or antidepressant medication: the habit of rumination can maintain depressive symptoms despite otherwise effective treatment.
Qualitative research by Ciobotaru et al. (2024) provides rich insight into the lived experience of rumination. Participants described it as a kind of “mental theatre”, replaying painful scenes from the past in an effort to understand them, which instead fuels distress. Over time, this process depletes energy, motivation, and concentration, leading to fatigue and disrupted sleep.

For CBT practitioners, this raises a crucial question: if rumination sustains depression, should we target it more directly?
Introducing Rumination-Focused CBT (RF-CBT)
Traditional CBT has a strong evidence base and remains the first-line treatment for depression and anxiety. However, standard CBT typically addresses rumination only indirectly, by challenging negative thoughts or modifying behaviours.
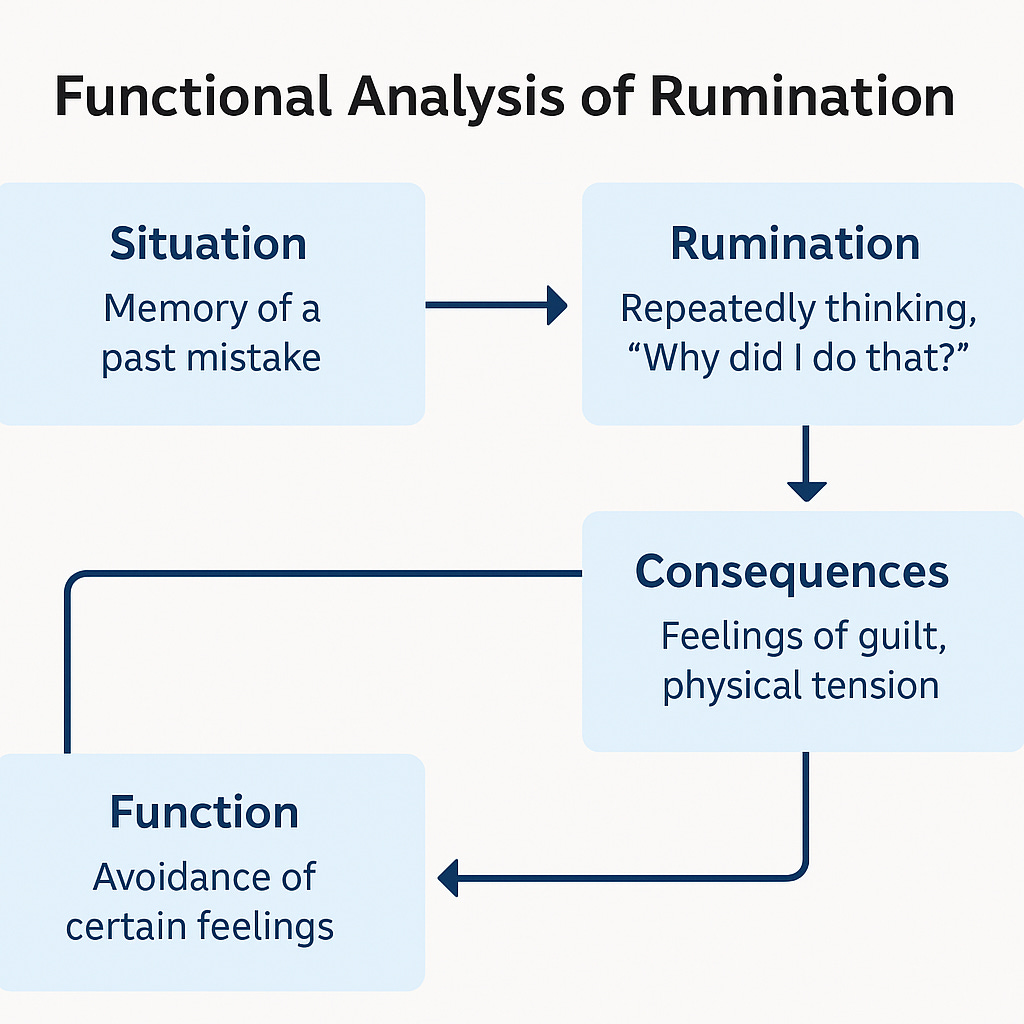
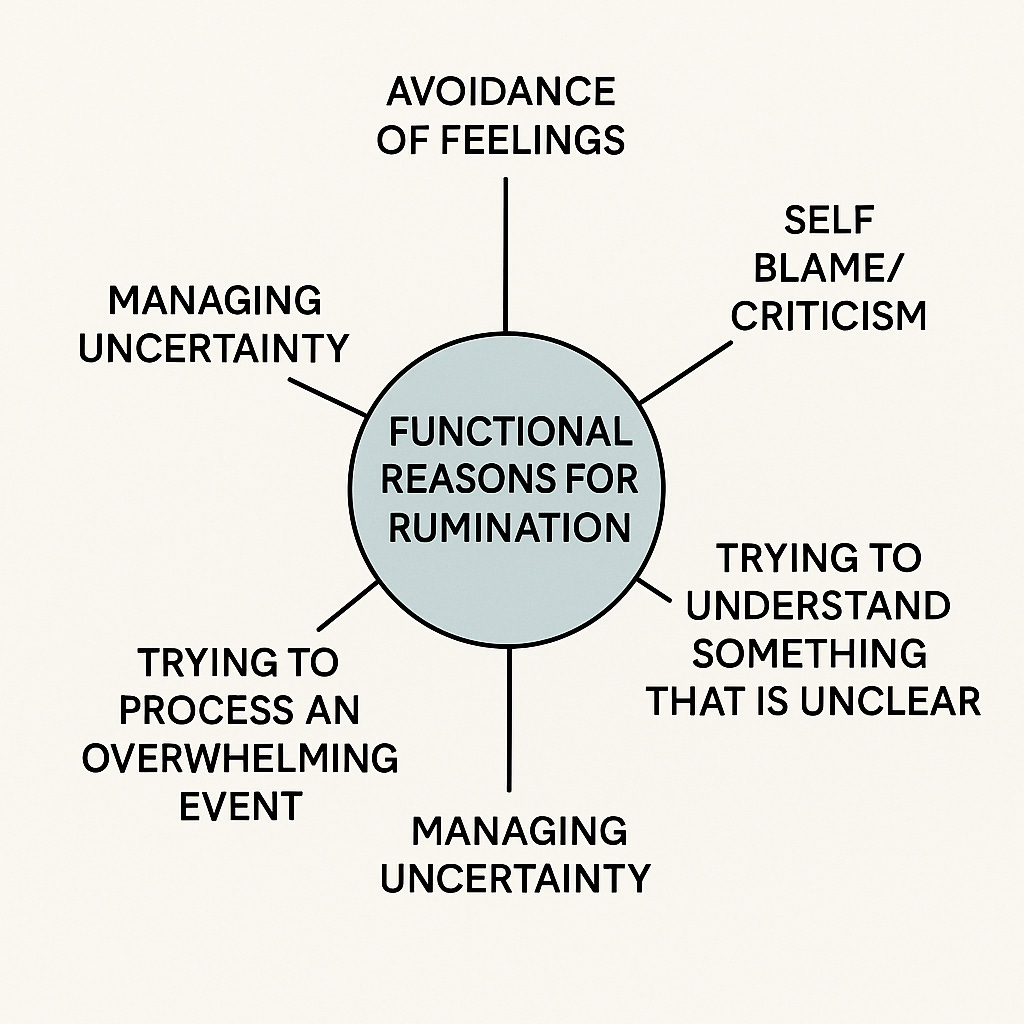
Rumination-Focused CBT (Rf-CBT) was developed to go a step further. It places rumination itself at the centre of treatment, aiming to:
Identify patterns of unhelpful repetitive thinking, understanding the functional reasons for rumination
Disrupt habitual rumination loops
Replace them with more constructive, flexible thinking styles
As Umegaki et al. (2021) note, Rf-CBT helps individuals shift from maladaptive to adaptive modes of processing, turning reflection into problem-solving rather than paralysis.
Early research is promising. Moeller et al. (2019) found that after 12–16 sessions of Rf-CBT, participants experienced significant reductions in depressive symptoms, particularly in cases where standard CBT had been less effective. This suggests that explicitly targeting rumination may improve treatment outcomes for persistent depression.
The Rumination and Worry Program: Making Rf-CBT More Accessible
Building on these ideas, Joubert et al. (2023) developed the Managing Rumination and Worry Program: an online adaptation of Rumination-Focused CBT.
This programme teaches participants to:
Recognise when they are ruminating
Understand the triggers and functions of rumination
Practise strategies to disengage from unhelpful mental loops
Research by Upton et al. (2025) supports its effectiveness, showing that repetitive negative thinking (including both rumination and worry) reduces significantly over treatment. Interestingly, baseline levels of rumination predicted how much improvement participants experienced, reinforcing rumination as both a key symptom and a treatment target.
Looking Forward: The Future of Rf-CBT
Rumination is a common, trans-diagnostic process that cuts across depression, anxiety, and trauma-related difficulties. While traditional CBT remains effective for many, it may not fully address repetitive negative thinking in all clients.
Rf-CBT offers an important addition to the therapist’s toolkit, a way to directly target the thinking styles that maintain distress, particularly in clients who feel “stuck” despite prior therapy.
As our understanding of cognitive and neurobiological mechanisms deepens, therapies like Rf-CBT show how evidence-based practice can evolve — refining general approaches to meet specific needs.
Tell us, do you work directly with rumination?
Author: Max Roberts


Really great article, Rumination comes up for almost all of my clients. I would be really interested to see an article/training on the intervention strategies involve in RF-CBT. I tend to use a mix of CBT and ACT approaches to manage the symptoms of rumination.